Anaesthesia, although very safe, must be well planned. It is important to spend time with the anaesthetic team talking through some of the problems these children have that may complicate the use of anaesthesia. These issues may include:
- • Short Necks
- • Limited jaw and neck movement
- • Thick tongues
- • Airways obstructed by storage material
- • Floppy tracheas (windpipes)
- • Inefficient breathing. Abnormalities of the spine and ribs can limit the patient’s capacity to breath and fully expand their lungs.
Anaesthesia in young children should always be performed by a paediatric anaesthesiologist who has experience with difficult airways and skeletal dysplasias. The neck of these children may be somewhat lax and could be more prone to injury during intubation. Also, the storage material may interfere with the placement or removal of the tube. Very small endotracheal tubes may have to be utilized. However, under the correct supervision, surgeries most often go very well.
In older ML patients a safer approach to passing a tube into the airway (intubation) might be by numbing the mouth and throat with local anaesthetic and passing a fine flexible telescope into the wind-pipe (trachea) while the person is a wake and co-operative. Then an endotracheal tube can be passed over the telescope and the airway secured before the person is put to sleep.
The Australian MPS Society has a wonderful booklet called MPS and Anaesthesia it can be ordered by contacting them on their website.

Carpel tunnel syndrome is very common in MLIII. The clinical signs are sensations of “pins and needles” in the fingers, loss of feeling and wasting of the muscle at the base of the thumb. The hand could also be weak.
Some children will never complain of pins and needles. They may have had symptoms for a long time, but do not understand what is meant when questioned regarding pain because of the constant nature of the pain sensations they have been experiencing. You may notice that the child will not be aware of hot and cold. This is an indication that perhaps there is nerve compression in the carpel tunnel.
To determine if the child has this compression, nerve conduction tests are necessary to check for nerve damage. This test feels like small spiders running up the hand and lower part of the arm. Most children tolerate this test really well but it has been noticed there can be moderate pain near the end of the testing process.
Carpel Tunnel has been diagnosed in an ML III child as young as 4 years of age.
Many doctors will doubt that young children have this condition. You will need to be persistent and explain that your child has a storage disorder and this is a frequent finding associated with the condition.
The median nerve travels from the forearm into your hand through a “tunnel” in your wrist.
The bottom and sides of this tunnel are formed by wrist bones and the top of the tunnel is covered by a strong band of connective tissue called a ligament.
This tunnel also contains nine tendons that connect muscles to bones and bend your fingers and thumb.
These tendons are covered with a lubricating membrane called synovium which may enlarge and swell under some circumstances.
If the swelling is sufficient it may cause the median nerve to be pressed up against this strong ligament which may result in numbness, tingling in your hand, clumsiness or pain.
Another important aspect to consider with Carpel Tunnel in these children is that although the carpel tunnel will be tight and will be compressing the nerves travelling through this area, compression can also be found either higher into the wrist area or down into the palm of the hand. It is important to explain this to your doctor and ask him to look further than the Carpel Tunnel. Remember, your child has a storage disease that affects the entire body.
There is no real documentation on CNS involvement in ML III, it is thought that these children do not have CNS involvement, but there are several children around the world who exhibit this problem.
If your child is complaining of pins and needles in their arms and legs it is important that an MRI is done and it is read by a doctor who has a very good understanding of ML. If an MRI is done of the brain the doctor will see white patches in the brain this is storage material and can be mistaken for other disorders. Once again make sure you tell the doctor you child has a storage disease.
There are no easy answers to this problem in ML III, and requires further research.
If your child has a heart problem (refer to the Heart section later), you will need to ensure that before any dental treatment is carried out such as scaling, fillings or dental extraction, they may need to take prophylactic antibiotics. The mouth has certain bacteria that may get into the bloodstream and cause infection in the heart valves.
If teeth need to be removed under anaesthetic, this should be done in a hospital situation under the care of an experienced anaesthetist.
Some ML III children do require dental extraction of their baby teeth as they tend not to fall out. Others will have problems with new teeth erupting through the gums and this process can be assisted by the Dentist under hospital procedure.
There have been no studies completed in the area of dietary needs of children with ML III, but due to hip deterioration it is important that weight is controlled and managed with a healthy diet.
Once your child has been diagnosed with ML you will need to work with your Paediatrician or Genetic Specialist to build a team of Doctors who will help you manage the many complications of ML.
Some of these Doctors could be:
- • Cardiologist
- • Dentist
- • Orthopaedic specialist
- • Endocrinologist
- • Dietician
- • Eye Specialist
- • Ear Nose and Throat Specialist
- • Neurologist
- • Spinal Surgeon
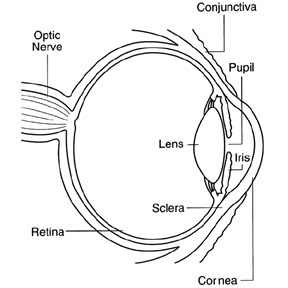
ML children need to have regular eye checks to look for clouding of the cornea.
The cornea is the eye’s outermost layer. It is the clear, dome-shaped surface that covers the front of the eye.
Because the cornea is as smooth and clear as glass but is strong and durable, it helps the eye in two ways:
1. It helps to shield the rest of the eye from germs, dust, and other harmful matter. The cornea shares this protective task with the eyelids, the eye socket, tears, and the sclera, or white part of the eye.
2. The cornea acts as the eye’s outermost lens. It functions like a window that controls and focuses the entry of light into the eye. The cornea contributes between 65-75 percent of the eye’s total focusing power.
In ML children, the corneas may become cloudy due to build up of storage material. If corneal clouding is severe, it may reduce sight. Additionally, light may come into the eye unevenly, especially bright lights. Thus sunglasses in bright lights may help. And, if vision is reduced, you should make sure there is appropriate lighting and avoid dim lights. For significant corneal clouding, causing limitation in vision, a corneal transplant may be considered.
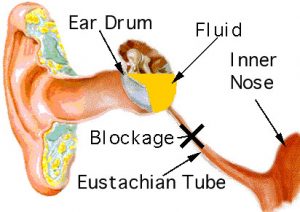
ML III children can suffer from many ear infections in their early childhood.
When the eustachian tube doesn’t operate correctly, due to anatomical problems, injury or swelling, new air is not able to reach the middle ear.
The body will remove the air from the middle ear and this creates a vacuum (negative pressure). When the pressure is mild, this may cause stuffiness or pressure in the ear.
When the pressure increases, the body senses pain. When the pressure remains for a period of time, the body replaces the vacuum with fluid. The fluid behind the eardrum can lead to problems with hearing loss and ear infections. If this negative pressure persists, fluid from the lining of the middle ear will build up and in time become thick and like glue. Hence the condition known as “glue ear”
Ventilation tubes (grommets, PE tubes) are frequently employed in the ML III population to manage chronic serous otitis media, or recurrent otitis media not responsive to medical management. Each child needs careful evaluation by an ENT specialist, and if surgery is recommended, patients should see the anesthesiologist (anesthetist in NZ, UK) beforehand to ensure that the risks associated with anesthesia have been addressed and minimized.

Children with ML III may grow to between four foot six inches (140cm) and five feet (152cms), but once again there is a huge variation. Some ML III children are similar in size to MLII
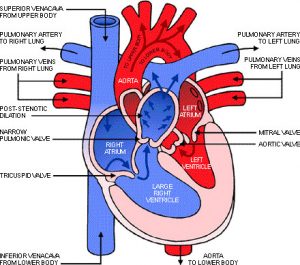
Heart murmurs will be heard by the doctor if your child has valves that have become damaged by storage material. Usually at this time your doctor will ask for an echocardiogram to be done. An echocardiogram is an ultrasound of the heart, much like the screening done when babies are in the womb. This allows the doctor to see what is happening to the heart
In ML III it is usually the Aortic and mitral valves that are causing problems, as the storage material builds up the valves become thickened and do not close off correctly.
The heart has four valves that open and close to keep blood flowing in the right direction through the heart.
The aortic valve connects the left ventricle to the aorta, which then allows blood to circulate to the rest of the body.
The mitral valve connects the heart’s upper-left chamber, the atrium, to the heart’s lower-left chamber, the ventricle.
When the valves do not function properly, amounts of blood may flow backward in your heart. This means that blood is not flowing as efficiently through the heart and to the rest of the body.
Storage of lysosomal material may weaken or thicken the valves, creating leakage around the valves. Treatment depends on the severity and progression of the valve’s leakage. It is possible that the leakage may not cause any problems; however it may cause fatigue and shortness of breath that may require surgery to repair or replace the valves.
During the winter months some ML III children get chest and respatory infections that require broad spectrum antibiotics. Many parents find the benefits of keeping their children on low dose antibiotics during these months to prevent infections setting in.
If your child has a cold or cough that does not seem to be getting better, you should seek medical advice.
Variation in IQ is considerable. Some children have normal intelligence, but some will have a learning disability which could involve short term memory loss. The reason for this is the continual build up of material being stored in the cell.
These children learn by repetitive teaching, and will require the services of special education, or teacher support time in mainstream education. To achieve the best education possible many of these children have IEP’s (Individual Education programs) which allows them to learn at their level.
An example of how the gap widens is seen in one ML3 young adult who is 23 years old. His learning level is 9 years of age and his reading level is 6 years of age, but he has an amazing memory for anything relating to sport. Early intervention was not part of this young mans life due to a late diagnosis of age 6. The informative years were lost and so the gap continued to grow over time.
It is important that a policy of early intervention be followed with the education of these children. Proactive education for these children will give access to necessary tools and materials and will increase a positive learning atmosphere and provide a guide base for each new teacher in your child’s future.
This requires that parents must become advocates for their children in fighting for services, therapies, and educational assistance. Laws and resources differ across the world, so it is important to learn about intervention services where you live.
Waiting and then establishing a reactive IEP will lose valuable time in your child’s overall education.
An example of what early intervention can do is seen in an 18 year old girl who was diagnosed at 2 years of age, by age 3
Those with ML III can live well into adulthood, some being supported at home others living independently, or in supported living arrangements.
There are a small number of ML III children who are severely affected and do not have a long life expectancy. It is important to note the wide range of individual abilities as our young adults mature. Parents should be prepared to understand the diversity and range of their ML III child, so they can help prepare a better future for their child.
Living with a child with ML III can certainly be a challenge, but also a joy. As parents of these very special children you will spend many hours learning everything there is to know about this disease, and over time you will become an expert in advocating for the best possible health care and Education available. It is important that parents actively have respite time away from their children to “re-charge” their batteries. You should not feel guilty about this but actively use this time as a tool to maintain your own energy levels and thus be a better advocate in the long term for your child.
One of the best gifts you can give your child is the gift of your own health as the caregiver and parent.
You may also wish to discuss the long term implications of care and funding for your child with your own legal adviser in the event that your own health or your pre-mature death will not allow you to continue caring and advocating for your child. There are many tools such as Trusts and Life Insurance that can be put in place to secure the long term future of your child.
Another useful tool is an Enduring Power of Attorney that can allow you to speak on behalf of your adult children for such things as health care, money management and rights to social security benefits. (In the United States it is referred to as Durable Power of Attorney and will differ from Country to Country)
Secondary Metabolic bone disease is very new to ML II and III. Very few doctors know about this and those that are introduced to it often state that this treatment will not work in ML.
The reason they say this is that once again bone disease in ML is not well understood and is often likened to Hurler disease.
The following information is written by the family who went through the first clinical trial with their two children and should be used along side the Medical paper, The Osteodystrophy of Mucolipidosis type III and the effects of intravenous Pamidronate Treatment, and Protocols for Use of Pamidronate, which can be downloaded as an Adobe PDF file.
Permission has been kindly given to us by Kluwer Academic Publishers who hold the copy rights.
(Kluwer Academic Publishers has merged with Springer-Verlag; the two publishing companies are now operating under the joint Springer brand. As a result, this Kluwer website has been redirected to springeronline.com)
Patients suffer to varying degrees the following complications.
- • Stiffness of hands and shoulders
- • Claw hand deformity
- • Scoliosis
- • Short stature
- • Low iliac wings, shallow acetabular fossa
- • Erosion of the femoral heads
- • Valgus deformity of femoral neck
- • Underdevelopment of posterior elements of dorsal spine
Dysostosis multiplex
- • Skull: calvarial thickening, premature suture closure, shallow orbits, abnormal tooth spacing, J-shaped sella
- • Spine: anterior hypoplasia of lumber vertebrae, kyphosis
- • Long bones: shortened, wide diaphyses, irregular metaphyses, poorly developed epiphyseal centres
- • Clavicles: short, thickened, irregular
- • Ribs: narrow at vertebral ends, flat and broad at sternal ends
- • Phalanges: shortened, trapezoidal in shape, widened diaphyses
What is happening to the bones of ML Children?
We all have cells that lay down new bone and cells that break down old bone; this is an on going process in all of us.
The cells that lay down new bone are called Osteoblasts and the cells that break down old bone are called Osteoclasts.
In children with Mucolipidosis type II & III the Osteoclast activity is extremely elevated and the osteoblast activity extremely low. So in effect ML children actually break down more bone than they lay down.
The nature of the bone pathology is that bones are extremely brittle and crumbling. Some degree of fracturing around the joints is inevitable from time to time. Each episode of fracturing and crumbling results in considerable pain and in some cases a loss of mobility.
An example of elevated osteoclast activity is seen in this example below.
The Normal range for bone turnover is <120 and is appropriate for age and sex.
Sibling one
| Time (months) | Alkaline Phosphatase |
| 0 | 256 |
| 6 | 187 |
| 12 | 156 |
You can see from here that sibling one at 18 years of age had extremely elevated bone turnover prior to treatment. These results are 6 monthly intervals where you can see a drop in bone turn over.
At four years of treatment you can see that the Osteoclast activity has dropped considerably.
| Date | Alkaline Phosphatase |
| 8/4/2004 | 93 |
| 5/5/2004 | 89 |
| 2/6/2004 | 90 |
Sibling two was considerably worse and was also going through puberty at the commencement of treatment.
Once again the Normal range is <250 and is appropriate for age and sex
Sibling Two
| Time (months) | Alkaline Phosphatase |
| 0 | 453 |
| 6 | 316 |
| 12 | 237 |
After four years of treatment you can see once again that Osteoclast activity has been reduced.
| Date | Alkaline Phosphatase |
| 8/4/2004 | 95 |
| 5/5/2004 | 89 |
| 2/6/2004 | 93 |
Pamidronate is one of the many Bisphosphonates available to treat pain and bone disease. It is also known as (Pamisol /Aredia), and is well known in the treatment of Osteogenous imperfecta (Brittle Bone Disease)
When Pamidronate is used, the Osteoclast (bone reabsorption cells) activity is decreased allowing the Osteoblast (laying down of new bone) activity to take over, and so increase bone density and repair some of the bone damage.
In these two young people it was found though bone biopsies that the Perosteal surface (hard outer layer of bone) was not being changed by Pamidronate, but at the Endosteal and Trabacular surfaces (soft internal parts of the bone) there was significant change in bone density after 12 months of treatment.
Pamidronate in Mucolipidosis is given through IV at monthly intervals and has not been trialled orally. The reason for this is that ML children can have stomach problems with many different kinds of drugs.
Most children will suffer some of the following symptoms in the first 2 infusions.
Flu like symptoms which include –
- • Fever
- • Nausea
- • Vomiting
- • Headaches and body aches and pains
These symptoms usually occur following the 1st infusion within 12 – 24 hours and subside within 48 hours. Some children who have commenced treatment in the United States reported body aches and pains which lasted for up to 7 days with the first infusion. These were managed with over the counter pain relief.
With subsequent infusions these symptoms do not usually occur but if they do it is to a lesser degree. Ibuprofen (Nurofen) and Paracetamol (Panadol) can be used to relieve any side effects.
Some of the children using this treatment have been broken in slowly to reduce the side effects of treatment. For example commencing with a ¼ dose in the first infusion ½ dose in the second infusion and a full dose in the 3rd infusion.
It has been noted that the side effects are less and the child recovers quickly from the 1st infusion.
Why was this chosen as a possible treatment for Mucolipidosis?
The two children from New Zealand who commenced the Study had the following problems prior to treatment.
- • The older sibling at age 18 was suffering from significant hip and back pain, which was seriously compromising his quality of life, waking him from sleep and interfering with wheelchair transfers.
- • The younger sibling by age 12 was also suffering from significant, constant joint pain, mainly from the hips. This was accompanied by a dramatic deterioration in her mobility. By age 14 she was unable to walk and was wheelchair bound.
- • Many forms of analgesia had been used in an attempt to decrease their hip and back pain. These had all been unsuccessful.
- •It was thought that these children could benefit from this treatment that showed outstanding results in Osteogenesis Imperfecta.
Treatment was commenced on 20th August 2000 with very rapid improvements
- • 2 weeks after the first infusion both children reported they were pain free.
- • The older sibling had increased mobility and was able to do all his own transfers.
- • By 18 months of treatment he was able to stand and take four steps. He also has not had any chest infections since commencing treatment.
- • The younger sibling also showed dramatic improvement in mobility. By 3 months of treatment she was able to walk with a walking frame and later progressed to Crutches and being able to walk unaided.
- • Both siblings are now able to do many of their own day to day cares.
Bone Density Results during Treatment
Sibling One
| Scan Date | Age | BMD (g/cm2) | Z Score | Change % |
| 16/8/00 | 18.3 | 0.523 | -3.9 | ….. |
| 13/2/01 | 19.8 | 0.554 | -2.9 | 5.9% |
| 28/8/01 | 20.8 | 0.605 | -2.3 | 15.7% |
| 26/2/02 | 21.3 | 0.638 | -1.6 | 22.0% |
| 19/3/04 | 22 | 0.694 | -1.4 |
Sibling Two
| Scan Date | Age | BMD (g/cm2) | Z Score | Change % |
| 16/8/00 | 14.6 | 0.751 | -3.1 | ….. |
| 13/2/01 | 15.1 | 0.871 | -2.7 | 16.0% |
| 28/8/01 | 16.6 | 0.962 | -1.7 | 28.1% |
| 26/2/02 | 17.1 | 1.065 | -1.3 | 41.8% |
| 19/3/04 | 18 | 1.209 | 0.1 |
You can see that after four years of treatment bone density continues to increase.
What are the first steps to take leading up to treatment?
To create baselines from which progress of treatment can be monitored. The following tests are carried out prior to treatment
- • Dexa Scan – this will measure bone density
- • Full skeletal X-Rays with bone age taken on left wrist
- • Renal Ultrasound
- • Blood and Urine samples taken for Endocrine and Biochemistry value.
A full explanation for all these tests are explained in the Protocols which can be downloaded from ISMRD’s website
A screen for lysosomal diseases is undergone through a urine spot screen, which looks for the presence of accumulated storage material in the urine. However, some of the lysosomal storage diseases do not have positive spot screens. Or, more advanced spot screens have to be pursued. For example, many labs screen for Mucopolysaccharide build-up, but others screen for oligosaccharides. It is important to work with a medical professional that is knowledgeable in lysosomal diseases and screening to get an appropriate work-up. If screening comes back positive, doctors typically consider further testing based on the clinical presentation of your child. For many lysosomal disorders, this is done through a blood test or skin biopsy looking for a decrease in a specific enzyme. Typically, specific enzymes have to be ordered, thus a “panel” of lysosomal enzyme testing is not available.
A diagnosis of ML is made by showing that lysosomal enzymes are increased in the plasma of the blood. Because of the targeting defect in ML disorders, the enzymes are not in the lysosome, but are in the extracellular fluid. A ML disorder can be diagnosed by documenting an increase of lysosomal enzymes in the plasma of the blood. Further confirmation can be performed by looking at the enzyme activity of N-acetylglucosamine-1-phototransferase, which is decreased in individuals with ML. Other confirmation can be performed by looking for the specific gene changes (mutations) within this gene. Enzyme activity and mutation testing are not necessary to make the diagnosis of an ML disorder. However, if a family would consider prenatal diagnosis for a future pregnancy, this testing would need to be performed.
With the large variation in ML III it is difficult to determine to what degree and when mobility becomes a critical issue. Children can suffer with mobility problems from as early as 4 – 5 years of age. There may be a noticeable change of gait to their walk. Long distances will become more difficult to achieve and the ML child may need to stop often for breaks in walking.
Other children could onset with independent walking at the ages of 9 – 10 years. With the onset of puberty there is a noticeable change in mobility. A mark able slow down in the ability to move independently for long periods increases to 5 or 10 minute walks, difficulty standing for long periods of time.
Metabolic bone disease must be considered at this stage as a major factor in the decline of mobility in your child. Wheelchairs and scooters, walking frames, crutches should be discussed with your doctor who will refer you to the appropriate people for assessment.
It is also important for parents to understand how these issues will cause difficulty in the schools and be prepared to have an IEP that addresses the appropriate measurements that need to be completed in order for your child to have success in school.
With this wide range – the onset of mobility issues and difficulty in walking may not occur till later into your young adult’s lives. This is determined by how each individual is affected by the build up of storage from this disease.
Many children with ML III will have chronic pain, which will interfere with their mobility, sleeping habits and quality of life.
Joint pain in Mucolipidosis will not respond to conventional drugs as we are not dealing with soft tissue damage in this disorder. We are dealing with secondary metabolic bone disease. Please refer to Metabolic Bone Disease for solutions to management of the pain issues.
ML III is often not diagnosed in a child until around 4 – 6 years of age. During this time there are little to no signs of the disability.
One of the first signs that there is something wrong with your child may be the curling of the little fingers or stiff shoulder joints. He/she may start to walk or run differently from other children. Some children will also start to show signs of curvature of the spine (scoliosis); they may also have a barrel chest. All these symptoms need medical assessment.
Some children will also start to show signs of curvature of the spine; they may also have a barrel chest, short neck, roundness in lower cheek area. Legs my start showing signs of contractures. All these symptoms need medical assessment.
This is done by providing blood and Urine samples for analysis. Usually this is followed by a Skin Biopsy that is grown to fibroblast level where the level of enzyme activity can be looked at. This will give a true indication of which Lysosomal disease your child has.
By around age 9 it will start to become more noticeable that your child will be shorter than their peers, they may be unable to keep up with other children in the School playground. .
As the children get older there will be noticeable clawing of the hands. Some children will start having difficulty in putting their heals down when walking, this is due to contractures in their hips and knees becoming more evident, some will also start complaining of pain when walking long distances and begin holding onto their upper thigh, and needing to take rests more often. This is the time to start looking at wheelchairs and other mobility devices. The need to start protecting joints becomes more urgent at this age.
Over the years there have been many discussions in regards to physio-therapy / PT and splinting with no clear reasons why one should or should not do this.
While the children are young and the disease process has not really kicked in they run, jump and play just like any normal child, this in effect could be called physo. As they child gets older their joints start to become stiff and they begin to slow down, mobility becomes a problem.
Many therapists believe that they are able to straighten out legs and arms and increase movement by giving these children physo. What has not been well understood in ML is that these children are beginning to have significant bone loss and physo of any kind should be incredibly passive. Physio-therapy / PT should not cause the child any pain. One must take great care of all ML joints, to prevent significant joint damage.
The best kind of physio-therapy for these children is Hydro-therapy. The warm water relaxes all the muscles and allows the child to have very relaxing passive therapy. Also, being in the water takes all the weight off their joints. Excellent results can be achieved by this kind of therapy.
With the onset of puberty comes a major change in the chemical reactions within the body. This is normal for everyone. What this does though in ML is accelerate the rate at which some storage happens and also accelerates bone deterioration. This area has not been well understood or even recognised as something that plays a major roll in the deterioration and loss of mobility in ML III.
Through the bone studies carried out in New Zealand and Australia it has been reported by the families involved that around 9 – 10 years of age seems to be a critical time for ML III. Families reported that they were seeing their children deteriorate in mobility, quality of life, and an increase in pain.
Since the introduction of Pamidronate families in the United States are also pin pointing a marked change in their children from 9years of age.
The bones of the spine usually line up from the neck to the buttocks. Because of the bone abnormalities in individuals with ML, the bones (vertebrae) may not stack up evenly, causing the stack of bones to be slightly curved.
This is often referred to as kyphosis, gibbus, or scoliosis, depending on where the curve is occurring. This curvature may progress over time and may require treatment if severe.
Some ML III children who have this problem have had rods inserted to stabilize the area that has become unstable.
At present there is no cure for ML III. Many of the complications can be well managed by surgical procedures.
For ML II and ML III Pamidronate is now being used to treat Secondary Metabolic Bone Disease (please see Metabolic Bone Disease).